The 8 Reasons to Choose Visalia Hearing Center
Request a Callback
Would you like to speak to one of our hearing care professionals to discuss your hearing health challenges? Then simply complete this form and we’ll call you back shortly.
"*" indicates required fields
#1 - Focus on Audiological Best Practices
We continually strive to deliver the highest standards of hearing healthcare. Our Director of Audiology, Dr. Dan Finnegan, has been helping people to optimize their hearing for the past 15 years.
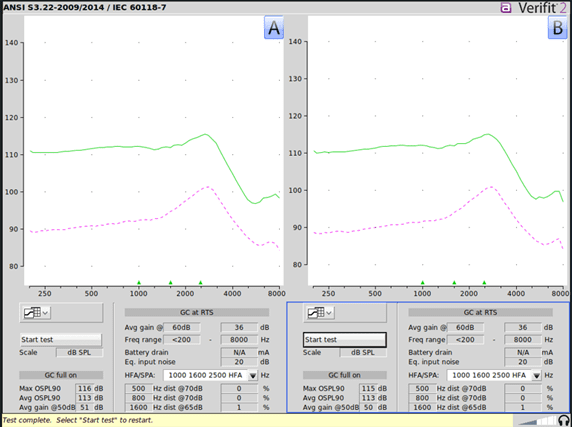
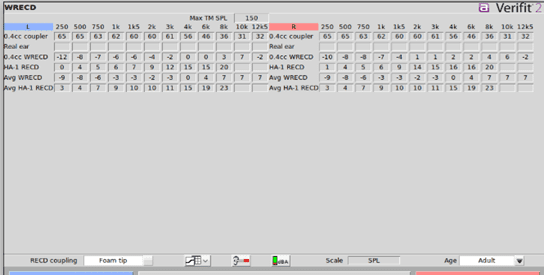
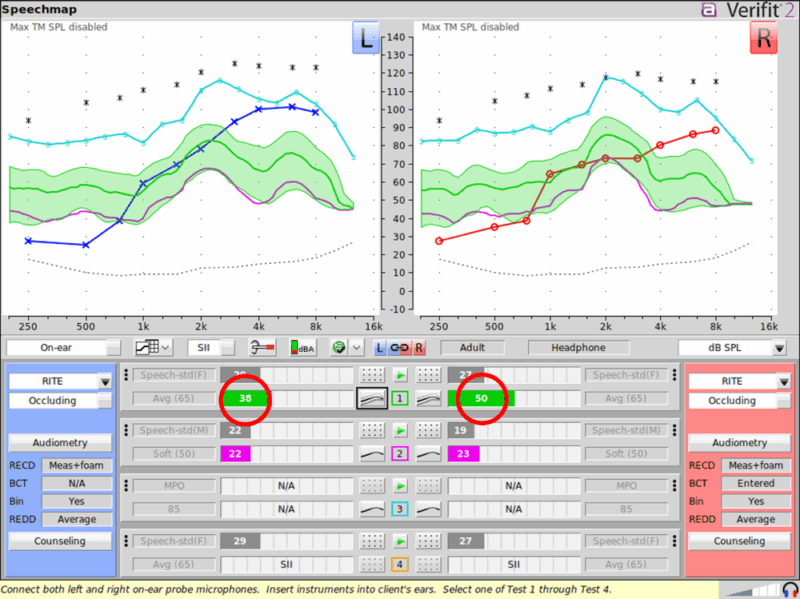
From voluntary Board Certification, a commitment to obtaining double the recommended continuing education units per year, having the latest in diagnostic equipment, and incorporating real ear verification and an aural rehabilitation program as part of their treatment plans, Visalia Hearing Center does not cut corner’s when it comes to patient care.
This means that you’ll not just be partnering with a local hearing professional, you’ll be partnering with a Board Certified Doctor of Audiology that is committed to excellence.
#2 - An Independent Business
Visiting a local independent restaurant offers a different experience than dining at a chain, and the distinction is even more pronounced in hearing healthcare.
Most chain hearing aid stores focus on a model that prioritizes the quantity of patients seen, applying ‘one-size-fits-all’ rules for their providers and limiting time with the people they’re trying to help—all aimed at growing the pockets of shareholders based thousands of miles away.
Our approach is very different: we only win when you win. Our independence ensures we can make the right decision in the moment, always in your best interest, with your investment reinvested locally.
#3 – Warm, Friendly and Accessible Location
We’ve all visited locations where the parking is a nightmare, you have to walk 100+ yards in 100-degree heat and finally be met with a flight of stairs to climb.
This isn’t the case with us. With convenient parking, easy access, comfortable seating and a warm yet professional atmosphere, your experience with us will be enjoyable from start to finish. This is hearing healthcare with a big heart and soul.
#4 – Here for the Long Haul
Hearing care is a lifelong journey. Once you find the right partner, you want assurance that they’ll remain by your side. As an independent practice who is planning for decades, not years, you can trust that our team is committed to fulfilling our long-term promises and always prioritizing your best interests.
#5 – Helping You to Choose The Right Hearing Technology
If you go to a Honda dealership, you can bet they’ll tell you a Honda is exactly what you need—Honda makes the best cars, after all.
The same is often true of franchised hearing aid locations; they usually work with just one manufacturer, meaning everyone receives the same solution, regardless of whether it’s the best choice for their individual needs. But as a true independent practice, Visalia Hearing Center takes pride in providing solutions across all six major hearing aid brands.
Very few clinics can say the same. Success with hearing aids requires both a skilled Doctor of Audiology and the right tool for the job. Current patients at Visalia Hearing Center know, and future patients can rest assured, that you’ll get exactly that here.
#6 – The Ear-Brain Connection: Taking Action
There’s been a lot of recent discussion around untreated hearing loss and its impact on cognition. The rumors are true, and that’s why Visalia Hearing Center has integrated state-of-the-art Cognivue Cognitive Screenings into our process.
Many hearing aid providers talk about the importance of hearing for cognitive health but fail to measure, assess, or monitor this connection—or to make an appropriate referral if changes occur, we do.
#7 – Timing is Everything
Three of the biggest frustrations with today’s insurance-based healthcare are: the long wait to book an appointment, extended waiting room times, and, after all that waiting, a rushed provider visit that barely lasts 10 minutes. Our approach is the opposite. Every appointment is scheduled within two weeks, over 90% of Dr. Finnegan’s patients are seen within five minutes of their scheduled time, and we often hear from patients, “This is the most time any doctor has ever spent with me.”
#8 – Qualifications Matter
Patient choice is important. In hearing care, you can take a do-it-yourself, over-the-counter (OTC) approach, work with a licensed hearing aid retailer, or choose to see a Doctor of Audiology. If education and training matter to you, a Doctor of Audiology is the choice you want. Since the person fitting your hearing aid plays a more significant role in your success than the device itself, it’s crucial to work with the most qualified team. At Visalia Hearing Center, a Doctor of Audiology will oversee your care every step of the way.
From Frustration to Freedom
You’ve tried hearing aids before. They didn’t work. That doesn’t mean you can’t hear better.
Many of our patients come to us after disappointing results elsewhere. One patient, on his third pair of name-brand devices, described them as “lousy” – until we showed him what real audiologic care looks like.
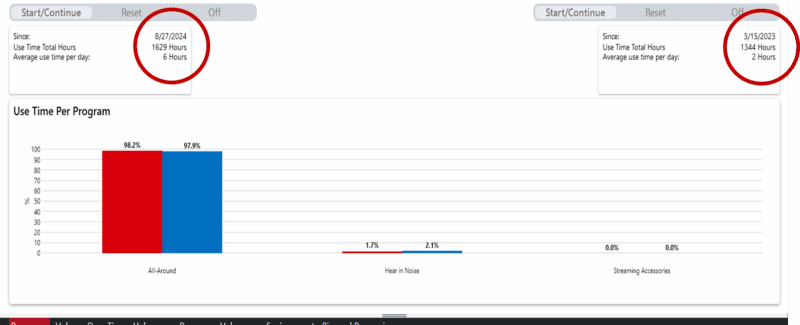
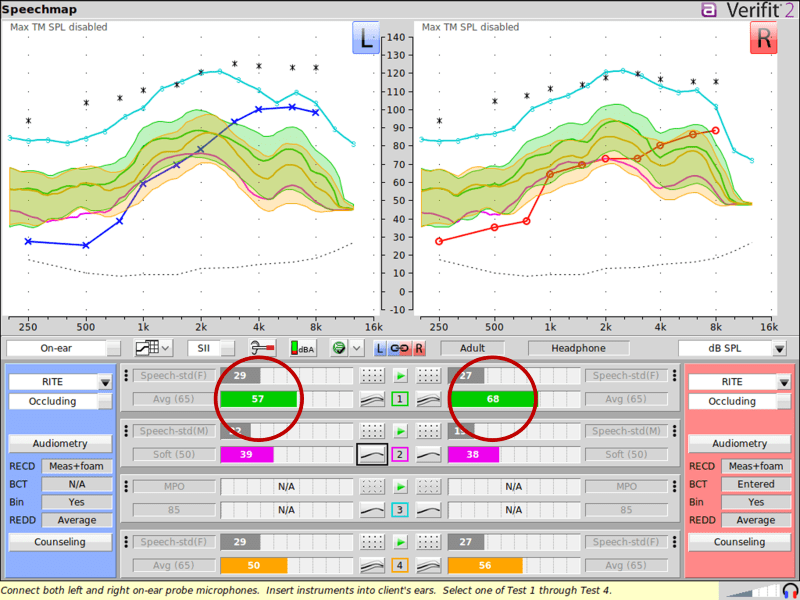
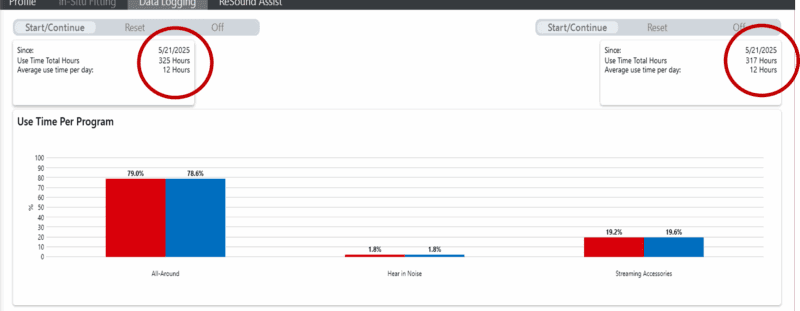
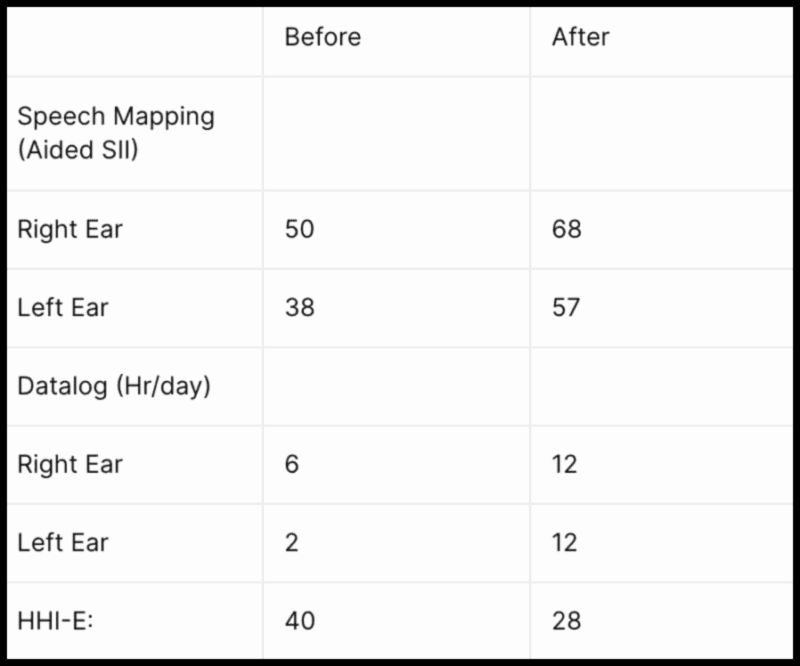
We performed a comprehensive analysis using tools most clinics don’t offer: QuickSIN, ACT, Speech Mapping, and Real Ear Measures. We didn’t recommend new devices. We optimized what he already had. Now he’s hearing his spouse again, enjoying TV with clarity, and wearing his aids all day, every day.
It’s not about the hearing aids. It’s about who’s programming them.